Long-term efficacy and safety of elamipretide in patients with Barth syndrome: 168-week open-label extension results of TAZPOWER
Authors: William R. Thompson, Ryan Manuel, Anthony Abbruscato, Jim Carr, John Campbell, Brittany Hornby, Frédéric M. Vaz, and Hilary J. Vernon
Journal: Genetics in Medicine (Link to article)
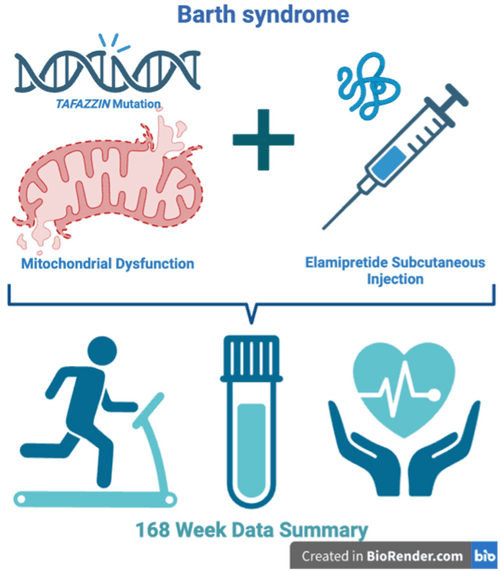
Barth syndrome is a disorder characterized by disruptions in mitochondrial function. Mitochondria are often called “the powerhouse of the cell” and when they are disrupted, less energy is produced by cells of the body. In Barth syndrome, problems in the heart, skeletal muscle, and immune system are caused by this mitochondrial dysfunction. One way to treat the symptoms of Barth syndrome is to provide a drug that can help restore mitochondrial function. In 2017, Stealth BioTherapeutics initiated a clinical trial called TAZPOWER to evaluate the effect of an investigational new drug called elamipretide. Elamipretide binds to a specialized lipid molecule called cardiolipin, which is located in the mitochondrial inner membrane, where it has an important role in many essential mitochondrial processes. The initial TAZPOWER trial was a 28-week, double-blind, placebo-controlled, randomized crossover trial where participants were randomly assigned to receive either elamipretide or placebo for 12-weeks and then crossed over to the other study treatment for 12-weeks after a 4-week washout period with no treatment (Understanding Clinical Trials). In this trial, participants received the study medication via a daily subcutaneous injection. After the initial 28-week period concluded, participants were offered the opportunity to continue receiving elamipretide as part of an open-label extension phase and results for weeks 36 and 72 were previously published (here and here, respectively). This week, researchers from Johns Hopkins, Kennedy Krieger, Amsterdam UMC and Stealth BioTherapeutics published a paper in the scientific journal Genetics in Medicine on findings from 168 weeks of elamipretide treatment for patients who remained in the open-label extension.
Findings: At the 168-week time point, the eight participants remaining in the open label extension were evaluated for the following primary endpoints: adverse events, laboratory values, vital signs, physical examinations, and electrocardiogram (ECG) measurements. Secondary endpoints evaluated included functional assessments including the 6-minute walk test, handheld dynamometry to test muscle strength, survey assessments of clinical symptoms and fatigue, cardiac function including left ventricular end-diastolic and -systolic volumes (i.e. amount of blood in the left ventricle pre- and post-contraction, respectively) and left ventricular stroke volume (volume of blood pumped out during left ventricle contraction) as well as the monolysocardiolipin:cardiolipin (MLCL:CL) ratio, which is a biomarker that estimates the amount of abnormal compared to normal cardiolipin in a small blood sample.
Primary Endpoints—Safety and Tolerability: All participants experienced treatment-emergent adverse events, with the most common being injection site reactions. Mean eosinophils/leukocytes ratios were elevated moderately from Week 12 onward and slight increases were also observed for hemoglobin levels through Week 144. Heart rate, blood pressure, ejection fraction and ECGs showed no statistically significant changes.
Secondary Endpoints—Functional Assessments: The researchers observed improvement over time for all participants and all endpoints from baseline in the open-label extension who had assessments through Week 168. This included an increase in distance walked in the 6-minute walk test, improved clinical and fatigue survey scores, SWAY balance scores and the 5x sit-to-stand test. Clinically meaningful improvements in left ventricular end-diastolic and end-systolic volumes and left ventricular stroke volume were also observed. Finally, the researchers found the MLCL:CL ratio significantly decreased with long-term open label elamipretide treatment through Week 168. A high MLCL:CL ratio is a hallmark of Barth syndrome and a decrease in this ratio may serve as another indicator of improvement.
Take-Home Message: Although the 12-week elamipretide study for TAZPOWER did not meet its primary or secondary endpoints, improvements in functional endpoints were identified after 36 weeks in patients receiving elamipretide through an open-label extension (reported in a prior publication). This most recent publication reports that durable improvements in functional and cardiac endpoints were observed for participants who continued receiving elamipretide through the open-label extension for 168 weeks. Elamipretide was also generally well tolerated in the TAZPOWER study—consistent with the known safety profile of the drug—with injection site reactions being the most commonly reported adverse event. The researchers hypothesize that improvements were not seen immediately following the initial 12-week treatment period because it may be an insufficient treatment period to observe meaningful changes and/or improvements in the heart and skeletal muscle may require a longer period of treatment to take effect.



