Novel Coronavirus 2019 (COVID-19) Precautions
December 11, 2020
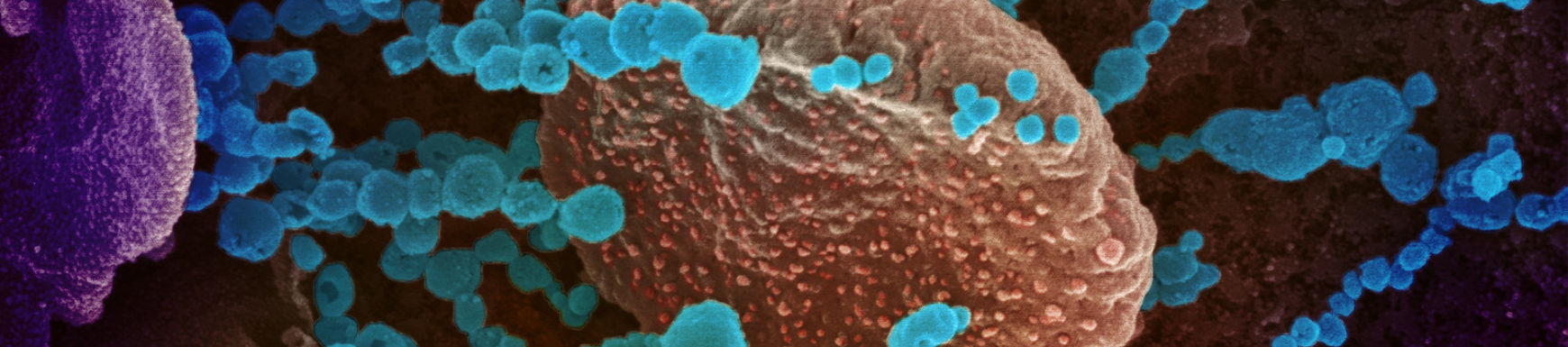
Human coronaviruses are a large family of viruses[i] which were first characterized in the 1960s[ii] . They are responsible for a substantial proportion of upper respiratory tract infections[iii].The novel coronavirus has been named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and the disease it causes has been named “coronavirus disease 2019” (COVID-19). This is a new virus in the coronavirus family. The virus that causes COVID-19 and the one that causes Severe Acute Respiratory Syndrome (SARS) are different from one another.
Symptoms
There are many similarities between COVID-19 and “the flu,” which is caused by the Influenza virus[iv].Both cause fever, cough, body aches and fatigue. Gastrointestinal symptoms (vomiting and diarrhea) have been reported[v] in at least one child with COVID-19. The symptoms can be mild or severe. Both viruses can result in pneumonia. Fatalities have occurred with both viruses.
Transmission
COVID-19 can be spread through person-to-person contact with large droplets from an infected person when they cough, sneeze, talk, and exhale. Studies suggest that COVID-19 may persist on surfaces for a few hours or up to several days. It can be spread through droplets that land on objects and surfaces. Generally, this is within a distance of 3 feet/ 1 meter. The flu and COVID-19 can be spread by an infected person for up to 2 weeks before symptoms appear.
Studies are underway to determine if COVID-19 can be transmitted through smaller particle droplets that spread over distances greater than 3 feet/1 meter from an infected person coughing, sneezing or talking. This is known as airborne transmission.
Prevention and Treatment
Both the flu and COVID-19 may be prevented by frequent, thorough hand washing, coughing into the crook of your elbow, staying home when sick and limiting contact with others who are or may be infected. Because someone may be infected but have no symptoms early on, social distancing is key to preventing spread of this pandemic.
A vaccine is available and effective in preventing or reducing the severity of infection with Influenza. There is no vaccine available at this time for COVID-19; it is estimated to take 1-2 years before a vaccine is available.
Neither the flu nor COVID-19 are treatable with antibiotics, which only work on bacterial infections. Antiviral medications can treat Influenza and can sometimes shorten the duration of the illness. Antiviral medications are currently being tested to see if they can address COVID-19 but at present there are no proven, effective antiviral treatments.
People with cardiovascular conditions such as Barth syndrome are at increased risk of disease severity with any respiratory illness. The American College of Cardiology has released COVID-19 Clinical Guidance For the Cardiovascular Care Team[vi].
Individuals with Barth syndrome are at risk of experiencing cardiac arrhythmia[vii]. Therefore, it is important not to take over-the-counter decongestants and multi-system cold remedies that contain decongestants before first consulting with the doctor.
Antibiotics may be prescribed for bacterial infections that can occur while fighting off some viral infections. If your doctor thinks respiratory symptoms could be helped by antibiotics and recommends a fluoroquinolone antibiotic, ask specifically about the risk of arrhythmias with these medications. The antibiotics in this class are: Avelox, Cipro, Factive, Levaquin, and Ofloxacin and can cause arrhythmias in some patients with cardiac issues.
It is important for patients with cardiovascular disease to remain current with all vaccinations. Ask specifically about getting the pneumococcal vaccine and influenza vaccines.
Barth Syndrome Specific Concerns
There are precautions for your loved one who has Barth syndrome during the COVID-19[viii] outbreak or anytime. Start by familiarizing yourself with standard Neutropenia precautions which exceed WHO and CDC precautions.
Neutropenia Precautions
- Have gloves on hand to use when needed
- Avoid crowded places; best to stay home to limit exposures to people who may be infected but do not yet have symptoms.
- Avoid interaction with people who are sick or have been recently sick
- Avoid person-to-person contact with others (6 feet/2 meters)
- Don’t share food, drink cups, utensils or other personal items, such as toothbrushes
- Wash raw fruits and vegetables
- Avoid touching surfaces that may have or would have been touched by someone in community or classroom or
- disinfect[ix] surfaces before touching (e.g., tables, desktops, doorknobs, light switches, handles, toilets, faucets, etc.)
- Avoid touching mouth and nose
- Wash your hands frequently[x] for at least 20 seconds
- Keep personal hand sanitizer[xi] available that is at least 60% alcohol
- If you plan to make your own, use the WHO-recommended formulations for Handrub solutions[xii].
- Wrap infants in two blankets, carry several clean blankets to change outer blanket when needed
- inner blanket/clean blanket
- outer blanket/barrier blanket
- Bathe when you get home
- Call the doctor with a fever of 100.4°F/38° or higher
- Call the doctor for advice with symptoms of illness
- Stay home when sick
Barth Syndrome is not classified as a primary mitochondrial myopathy. However, the defective biosynthesis of cardiolipin in Barth syndrome patients does result in mitochondrial dysfunction. Therefore, mitochondrial precautions should be observed with patients who have Barth syndrome. Below are additional recommendations provided by the Scientific and Medical Advisory Board of the United Mitochondrial Disease Foundation (UMDF) [xiii].
Respiratory viruses may lead to bacterial infections including ear, eye and sinus infections or even a secondary bacterial pneumonia. In some cases, respiratory viruses can be dangerous, and result in respiratory distress and the need for immediate medical attention. The risk of dehydration and subsequent organ failure has been noted in early reports, and as with other viral illnesses in mitochondrial patients, early administration of oral and intravenous fluids to prevent dehydration may be a very important part of effective treatment.
Be aware that relatively few children have been identified with COVID-19 disease, and so the impact on children with mitochondrial disease is unclear. If there are other family members attending school or attending a workplace in close proximity to other workers, keeping your child with a mitochondrial disease home from school must be supplemented by effective hand washing by all who come into the home and restricting all unnecessary contacts (other children, visiting relatives, etc).
A young infant with a mitochondrial disease and a fever should always be seen by a doctor, even if it seems like they just have a cold, as it may be COVID-19 disease, or influenza, which needs to be treated with the same degree of concern as would COVID-19.
Until we know more, it makes sense to see a medical provider if the illness causes a high fever, or a fever that goes away and then comes back. These can be signs of a bacterial infection including pneumonia, ear infections, and sinus infections.
Any sign of difficult breathing, unusual noises with breathing, not being able to drink liquids, severe coughing, extreme tiredness or constant fussiness in an infant or child is serious and requires urgent medical evaluation. Again, this is true for the mitochondrial patient regardless of a coronavirus pandemic.
A parent or caregiver who is uncomfortable with the condition should be taken seriously and be encouraged to seek medical care.
Additional Updates from UMDF
Other COVID-19 Precautions
Seek medical advice if you develop COVID-19 symptoms (fever, cough, trouble breathing)[xiv]
Call doctor if you or someone in your home has traveled from an area with widespread[xv] or ongoing community spread of COVID-19
Contact the school to inquire about available resources for a child who would be at high risk if exposed to COVID-19 (e.g. Hospital/medical homebound program)
Reviewers
Brian Feingold, MD, MS, FAHA: Medical Director, Heart Failure and Heart Transplant Programs, Associate Professor, University of Pittsburgh School of Medicine
Colin K. Phoon, MD: Associate Professor, Department of Pediatrics, Hassenfeld Children's Hospital at NYU Langone
References
[i] Coronavirus. WHO (Link)
[ii] Tyrrell DA, Bynoe ML. Cultivation of viruses from a high proportion of patients with colds. Lancet. 1966;1:76–77 (Link)
[iii] Kahn JS, McIntosh K. History and Recent Advances in Coronavirus Discovery. Pediatr Infect Dis J. 2005 Nov;24(11 Suppl):S223-7, discussion S226. (Link)
[iv] Maragakis LL. Coronavirus Disease 2019 vs. the Flu. Johns Hopkins Medicine Health, Infectious Diseases (Link)
[v] Coronavirus Disease-2019 (COVID-19) and Children, Frequently Asked Questions and Answers. CDC, NCIRD, Division of Viral Diseases (Link)
[vi] ACC President Message: ACC Issues COVID-19 Clinical Guidance for the CV Care Team. ACC (Link)
[vii] Spencer CT, Byrne BJ, Gewitz MH, Wechsler SB, Kao AC, Gerstenfeld EP, Merliss AD, Carboni MP, Bryant RM. Ventricular arrhythmia in the X-linked cardiomyopathy Barth syndrome. Pediatr Cardiol. 2005 Sep-Oct;26(5):632-7. (Link)
[viii] Coronavirus Disease 2019 (COVID-19) How to Protect Yourself. CDC (Link)
[ix] Coronavirus Disease 2019 (COVID-19) Clean &Disinfect. CDC (Link)
[x] When and How to Wash Your Hands. CDC (Link)
[xi] Show Me the Science- When &How to Use Hand Sanitizer in Community Settings. CDC (Link)
[xii] Guide to Local Production: WHO-recommended Handrub Formulations. WHO (Link)
[xiii] Scientific and Medical Advisory Board Position Statement: Coronavirus, Influenza and other Viral Respiratory Diseases in Adults and Children with Mitochondrial Diseases. UMDF. March 2, 2020. (Link)
[xiv] Coronavirus Disease 2019 (COVID-19) Symptoms. CDC (Link)
[xv] Coronavirus Disease 2019 (COVID-19) How It Spreads. CDC (Link)
Additional Resources
Barth Syndrome Foundation
Returning to School and Workplace Resources
-
COVID-19 Planning Considerations: Guidance for School Re-entry
-
COVID-19 Suite Landing Page
Resources separated into topic specific pages including health-related, scientific information by government agencies on a federal and state level, COVID-10 information in other language formats, telecommunity technology tips, schooling at home, planning tools for workplace and school reopening.
Frequently Updated -
School Decision-Making Tool for Parents, Caregivers, and Guardians
A tool is designed to help parents, caregivers, and guardians weigh the risks and benefits of available educational options to help them make decisions about sending their child back to school.
July 23, 2020 -
Links to guidance documents for schools and childcare programs.
Updated Frequently -
Information on protecting the rights of individuals students with disabilities when schools reopen
-
eSchool+ Initiative
Resources to track state and national school reopening plans and more.
Frequently Updated -
eSchool+ Initiative
Video Series including school-based healthcare, how to support students with special needs as they return to school, etc.
Frequently Updated -
Guidance for Return to School for Transplant Families
July 30, 2020 -
Solid Organ Transplantation (SOT) Summary Points for School Entry
In response to mounting questions from families and SOT providers, a group of PIDS pediatric transplant ID physicians in collaboration with specialists with expertise in infection prevention, public health, and transplant psychology, convened to construct an expert opinion consensus statement regarding key considerations that providers and families can use as a framework when considering individual risk and shared decision-making about returning to school (K-12) this fall.
July 30, 2020 -
SPAN provides COVID-19 fact sheets and resources to help families advocate for services and accommodations for their special needs child
Frequently Updated
Centers for Disease Control and Prevention (CDC)
-
CDC’s Health Alert Network (HAN) is CDC’s primary method of sharing cleared information about urgent public health incidents with public information officers; federal, state, territorial, tribal, and local public health practitioners; clinicians; and public health laboratories.
CDC’s HAN collaborates with federal, state, territorial, tribal, and city/county partners to develop protocols and stakeholder relationships that will ensure a robust interoperable platform for the rapid distribution of public health information.
-
Updates on CDC response efforts to the spread and disease impact of COVID-19
Frequently Updated -
Frequently Update
-
Frequently Updated
-
Frequently Updated
Food and Drug Administration (FDA)
-
Frequently Updated
Medical Societies and Journals
-
American Academy of Pediatrics (AAP)
H. Cody Meissner, M.D., FAAP, May 11, 2020 -
American College of Cardiology (ACC), March 6, 2020
-
American Society of Transplantation (AST), April 29, 2020
-
Pediatric Heart Transplant Society, May 12, 2020
-
Pediatric Infectious Disease Society
July 30, 2020 -
American Society of Microbiology (ASM), Regularly Updated
-
Joint Statement American College of Cardiology (ACC), American Heart Association (AHA) and Heart Failure Society of America (HFSA), March 17, 2020
-
Novel Coronavirus Information Center
Elsevier’s free health and medical research on the novel coronavirus (SARS-CoV-2) and COVID-19
Frequently Updated -
COVID-10 Resources
Frequently Updated -
The Lancet has created a Coronavirus Resource Centre. This resource brings together new 2019 novel coronavirus disease (COVID-19) content from across The Lancet journals as it is published. All of our COVID-19 content is free to access.
Frequently Updated -
A collection of articles and other resources on the Coronavirus (Covid-19) outbreak, including clinical reports, management guidelines, and commentary.
Frequently Updated
Patient Advocacy Groups
-
The primary focus of ACTION is to improve outcomes for ventricular assist device (VAD) patients. They also provide information for solid organ transplant (SOT) recipients.
The COVID-19 page provides a list of resources for these individuals.
Fact sheets include information for solid organ transplant (SOT) recipients, instructions for children about how to wear a mask, facts about how COVID-19 is different from the flue in English and Spanish, tips for talking to friends and family members and children about why it is important for your family to socially distance, COVID-19 and VADs, changes patients and families might expect when they visit the hospital AND MORE! -
Coronavirus (COVID-19): What People With Asthma Need to Know, July 16, 2020
-
COVID-19 and Pediatric Cardiomyopathy
World Health Organization
-
Situation Map
Frequently Updated -
Frequently Updated
-
COVID-19 Events as they happen
Frequently Updated -
Frequently Updated
Miscellaneous
-
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)
Frequently Updated -
COVID-19 resources for all facilities, including the NETEC webinar series, PPE use and conservation guidance documents, education and training resources, CDC and WHO guidance documents, preparedness resources, research on respiratory pathogens and airborne transmission, clinical guidance documents, documents on ambulatory PPE, and other research resources.
Frequently Updated -
Tourism and Coronavirus Disease (COVID-19)
Frequently Updated